Introduction
Blastic Plasmacytoid Dendritic Cell Neoplasm (BPDCN) is a rare and aggressive hematological malignancy. The diagnosis can be challenging because of its rarity and heterogeneity of initial presentation of the disease that commonly affects skin causing violaceous lesions, bone marrow causing cytopenias, lymph nodes, and central nervous system. Cases with isolated organ involvement have been reported, which poses more diagnostic challenges. BPDCN commonly affects older male patients, limiting the usage of intensive chemotherapy like regimens used for induction therapy for Acute Lymphoblastic Leukemia/Lymphoblastic Lymphoma or Acute Myeloid Leukemia before consolidation with stem cell transplantation (SCT) in first remission. Novel targeted therapies, like the recently approved Tagraxofusp, can provide less toxic disease control modality and bridge to SCT in fitter patients.
Case Presentation
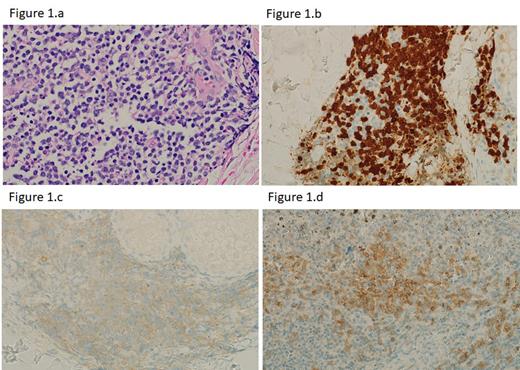
A 73-year-old male was referred to our hospital for evaluation of symptomatic pancytopenia (WBC 1,000/microliter, Neutrophils 71%, Hgb 96 g/dL, Hct 28%, Platelets 23,000/microliter). Bone marrow evaluation was non-diagnostic. Subsequently, he was on active surveillance to monitor his count during when the pancytopenia improved spontaneously over around five months-period. The patient began to develop bruise-like lesions over his nasal bridge, and scattered ones over his scalp and upper back. His blood count remained within normal limits. A punch biopsy of the upper back skin lesion showed infiltration with poorly differentiated medium-sized blasts (Figure 1.a). The malignant cells stained positive for CD123 (Figure 1.c), CD4, CD56, and TCL1 (Figure 1.b).
The patient was diagnosed with BPDCN. Given his age and poor functional status, he was not fit for intensive chemotherapy and was initiated on Tagraxofusp. Despite a brief improvement of the skin lesions, the lesions relapsed again and progressed further, requiring the addition of palliative corticosteroids. The patient required hospitalization for septic shock following the fourth cycle of therapy, which was, unfortunately, the cause of his demise.
Discussion
Recently, the 5 th edition of the World Health Organization classification of hematolymphoid tumors subcategorizes histiocytes/dendritic cell neoplasms into plasmacytoid dendritic cell neoplasms that encompasses BPDCN, Langerhans cell and other dendritic cell neoplasms, and histiocytic neoplasms. The immunophenotypic diagnostic criteria of BPDCN mandates either: expression of CD123 and one another plasmacytoid dendritic cell (pDC) marker (TCF4, TCL1, CD303, CD304) in addition to CD4 and/or CD56, or the presence of any three pDC markers and absence of all expected negative markers (CD3, CD14, CD19, CD34, Lysozyme, MPO). The recent breakthrough in novel CD123 antibody as a therapeutic advancement in offsetting the dismal prognosis of this disease has created more hope for patients with BPDCN, and to be able to receive curative SCT.
Although BPDCN carries a heterogenous disease course, we observed an unusual disease evolution in our patient before we reached the final diagnosis. Interestingly, we noticed a weakly positive expression of CD123 on the cutaneous lesion (Figure 1.c) and (Figure 1.d positive control), which is the main target of Tagraxofusp therapy. We hypothesize that the unfavorable response we observed with our patient was likely related to the weaker expression of the target CD123 antigen, which likely “bounded off” the anticipated molecular activity of Tagraxofusp in our patient. Further studies are warranted to confirm this observation.
Disclosures
No relevant conflicts of interest to declare.